If you’re dealing with persistent back or neck discomfort that worsens when sitting, standing, or transitioning between positions, you’re not alone. Many people who visit a chiropractor in Olathe describe a deep pressure or stiffness that builds throughout the day rather than a sudden injury. These patterns often overlap with issues discussed on our condition pages for neck pain, headaches, upper back pain, and low back pain, which serve as the primary resources for understanding those conditions in detail.
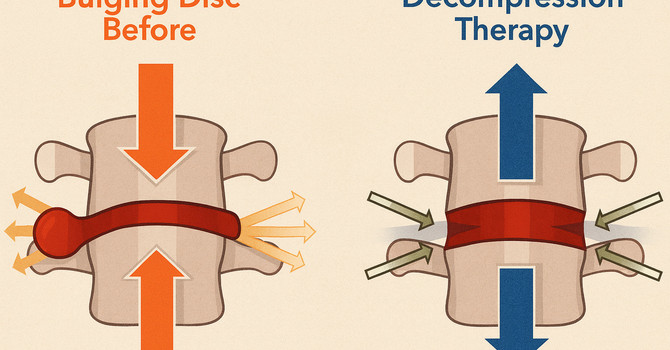
Spinal discs are designed to absorb load and allow movement, but prolonged pressure—especially from sustained sitting or static postures—can reduce normal disc fluid exchange and increase sensitivity in nearby joints and soft tissues. When that pressure isn’t relieved, discomfort can accumulate and feel harder to shake as the day goes on.
In many everyday situations, the spine experiences uneven loading. Sitting for long periods increases compressive forces through the lower back and neck, while limited movement reduces circulation to discs and supporting muscles. Over time, this combination can make discs less tolerant to stress, especially during transitions like standing up, bending forward, or turning the head.
People commonly describe patterns such as stiffness after long drives, aching in the low back after desk work, neck tightness with screen use, discomfort when standing after sitting, pressure that improves briefly with movement, soreness that worsens by evening, difficulty finding a comfortable seated position, or symptoms that fluctuate depending on posture rather than activity level.
Clinically, I often see movement-based intolerance rather than constant pain. Some patients feel worse with prolonged sitting, others with standing still, and many report relief when changing positions frequently. Morning stiffness versus evening fatigue patterns, sensitivity with spinal rotation, or symptoms that travel slightly into the shoulders, hips, or upper legs without clear injury are also common themes.
Spinal decompression is designed to address these mechanical stress patterns by gently reducing compressive forces on the spine. Rather than forcing movement, decompression focuses on creating a controlled unloading environment that may help discs rehydrate and reduce joint pressure. This approach is commonly discussed alongside chiropractic care when supporting patients who are already learning more about disc-related discomfort through our What We Treat resources.
Frequently asked questions patients often ask include:
How is decompression different from stretching? Decompression applies controlled traction to reduce spinal load rather than lengthening muscles alone.
Is decompression helpful if sitting makes my pain worse? It is often considered when sustained compression is a trigger.
Does decompression target the neck and low back? It can be applied region-specifically depending on the area involved.
How soon do people notice changes? Responses vary and often depend on activity levels and posture habits.
Is decompression the same as cracking or adjustments? No—these approaches work through different mechanical mechanisms.
If prolonged sitting or standing is contributing to ongoing spinal discomfort, understanding how load affects discs can help you make informed decisions. If you’re dealing with this type of problem, we can help. Call our Olathe chiropractic office at 913-735-6351, or click Schedule Your Visit to get started.
Dr. Ike Woodroof
Contact Me