Severe low back spasms can feel terrifying—especially when they come out of nowhere and make it nearly impossible to sit, stand, or move without sharp, stabbing pain. At Woodroof Chiropractic & Acupuncture, many patients in Olathe search for an Olathe chiropractor the moment these symptoms hit, and for good reason: early treatment helps prevent worsening disc irritation, muscle guarding, and long, painful flare-ups. This case highlights how a targeted plan using chiropractic care, spinal decompression, and hydromassage therapy can calm spasms and help patients walk, sit, and function again.
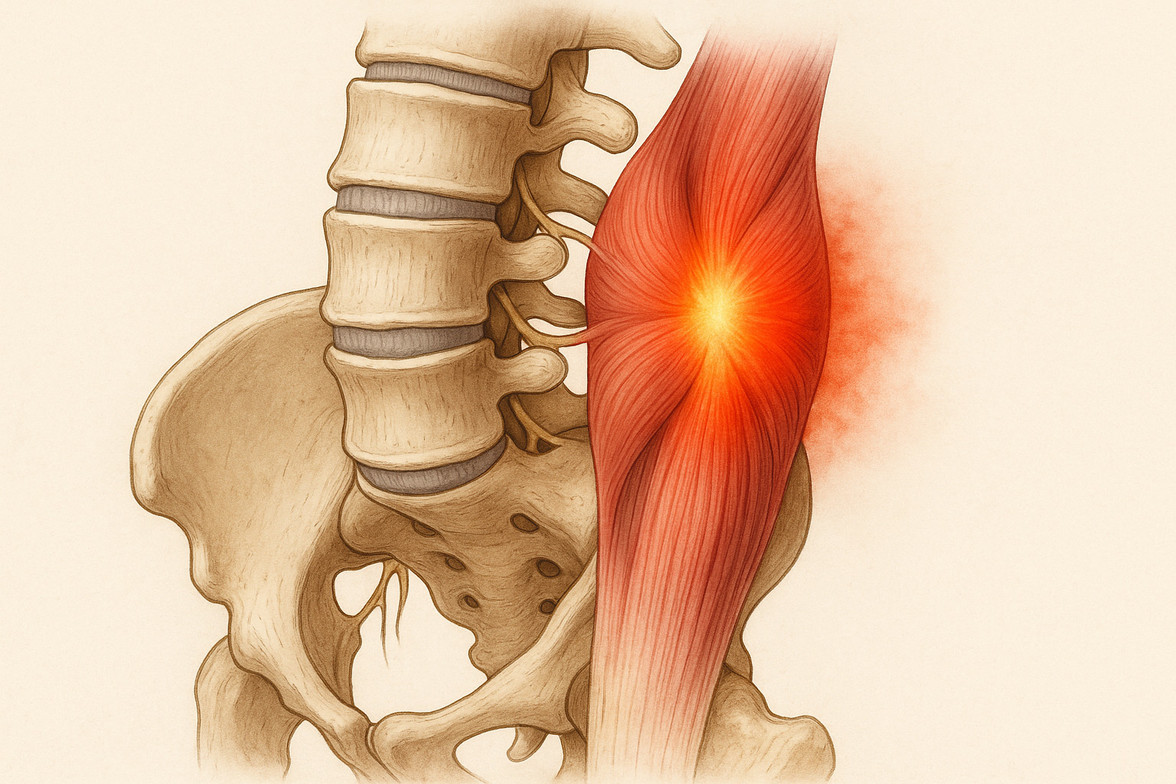
Back spasms often occur when an irritated lumbar disc, inflamed joint, or strained muscle triggers a protective “locking down” response. When the brain senses instability, it tightens the muscles to guard the area—which causes even more pain. This is why people with disc irritation often feel sudden seizing pain with simple movements like sneezing, bending, or walking up stairs.
Why this problem happens:
Lumbar discs can become irritated from compression, twisting, poor posture, or old injuries. When this irritation affects the annular fibers or internal structure of the disc, the surrounding muscles contract to protect the spine. This leads to sharp spasms, difficulty standing upright, and pain with weight-bearing. The lumbar joints at L3–L5 can also become fixated, further limiting movement and increasing pressure on the disc and surrounding nerves.
Common symptoms patients notice include:
• Sudden sharp pain after sneezing, twisting, or bending
• Low back muscles locking up or spasming
• Pain that increases when trying to sit upright
• Difficulty standing from a chair
• Pain radiating into the hip, low back, or buttock
• Needing to lie flat to get relief
• Increased pain when walking upstairs or bearing weight
• Feeling “crooked” or unable to stand fully upright
These are common patterns we also see on our low back pain and sciatica pages.
Clinical patterns I see in the office:
Many patients report pain that intensifies after sitting for too long or after standing in one spot. Others notice relief when lying on their back with their knees bent or shifting onto their right side. Often, they cannot tolerate lying face-down because of the pressure on the irritated disc. These patterns help guide us toward the correct diagnosis—typically disc irritation, annular tearing, or joint fixation rather than a major disc herniation.
In this specific case, the patient first experienced severe spasms in July 2024 after sneezing—so sudden that it required an ER visit and MRI. The imaging showed no disc herniation, but the clinical symptoms strongly suggested internal disc disruption. The pain resolved within a week, but nearly one year later the spasms returned (08/23/2025), this time triggered by simply walking upstairs. The patient arrived unable to sit, using crutches to walk, and could only stand or lie down with support. On examination, we found severe left-sided lumbar paraspinal spasm and joint fixation from L3 through L5 with pelvic imbalance. Pain increased with sitting, standing, or lying face-down—and decreased when lying flat or on the right side.
How chiropractic care helps:
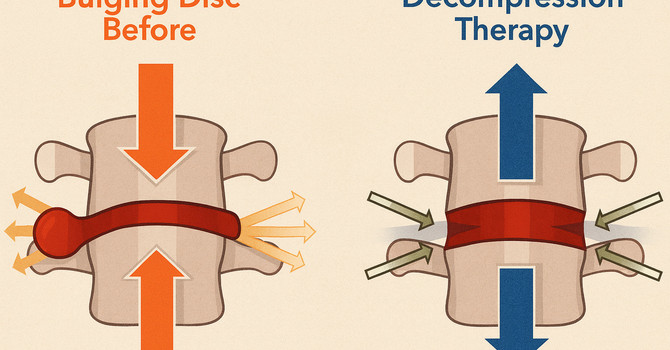
Gentle lumbar chiropractic adjustments restore movement to the restricted joints and reduce mechanical pressure on the irritated disc. Spinal decompression lowers intradiscal pressure, helping the annulus heal and reducing nerve irritation. Hydromassage therapy calms the protective muscle guarding so the spine can move without spasming. We often pair these treatments with a tailored exercise and stretch routine to improve stability, reduce flare-ups, and teach patients how to move safely at home.
Our treatment approach at Woodroof Chiropractic:
This patient began daily treatments for the first two weeks, including gentle lumbar adjustments, targeted decompression, hydromassage, ice/heat therapy, and positional coaching. As his symptoms improved, we tapered to 2–3 visits per week and added progressive strengthening, stretching, posture guidance, and sleep recommendations. Most patients—including this one—begin noticing improvement within the first few visits.
Progress and results:
Within 10 visits (08/27/2025–09/10/2025), this patient went from severe pain and inability to sit to nearly pain-free movement:
• Visit 1: 7/10 pain, unable to sit
• Visit 3: 3/10 pain, improved standing
• Visit 5: 2/10 pain, minimal tenderness
• Visit 6: 1/10 pain, moving comfortably
• Visit 9: transitioned to weekly maintenance
By the final visit, the patient could sit, stand, and walk normally, with significant reduction of muscle spasm and improved lumbar mobility.
Frequently asked questions include:
• Why do back spasms happen after simple movements like sneezing?
Because sneezing rapidly increases spinal pressure, which can irritate a vulnerable disc.
• Should I see a chiropractor for severe low back spasms?
Yes—gentle adjustments and decompression can reduce pressure and speed recovery.
• How long until I feel better?
Many patients notice improvement within their first few treatments.
• When is it serious?
If you cannot walk, cannot stand upright, lose bowel/bladder control, or have numbness in the groin, seek emergency care.
If you’re dealing with severe low back spasms or sudden back pain, we can help. Call our Olathe chiropractic office at 913-735-6351 or click Schedule Your Visit to get started today.
Dr. Ike Woodroof
Contact Me